Fagkronikk

Can physiotherapists timely detect patients at risk for delayed return to work after Total Knee Arthroplasty? Yes they can!
Fagkronikk/ Expert opinion piece.
Yvonne van Zaanen, Department of Public & Occupational Health, Amsterdam UMC, y.vanzaanen@amsterdamumc.nl.
Paul Kuijer, Department of Public & Occupational Health, Amsterdam UMC.
Fagkronikker vurderes redaksjonelt.
Expert opinion pieces are reviewed by Fysioterapeuten.
Physiotherapists play a crucial role in supporting patients’ recovery after total knee arthroplasty (TKA). One of the biggest challenges many face is regaining the ability to perform work-related activities, which are often physically demanding and require good knee function. Recent research highlights that the Work, Osteoarthritis, or Joint Replacement Questionnaire (WORQ), administered just three months after surgery, can identify patients who may experience limited work ability or a delayed return to work (RTW) (1). Detecting these patients early allows physiotherapists and healthcare teams to tailor rehabilitation programs and provide additional support, potentially improving long-term outcomes and helping patients reintegrate into their work lives more smoothly.
Using the WORQ to assess work recovery
The WORQ is a patient-reported outcome measure that focuses specifically on work-related knee activities (2, 3). It includes 13 common activities that place strain on the knee, such as kneeling, lifting, squatting, or working with hands below knee height. Patients rate their difficulty performing these tasks on a 5-point scale. Each activity is rated from 0, for extreme difficulty or not able to perform, to 4 which means no difficulty at all. The ratings of 13 activities add up to a score between 0 and 52, which is converted ((:52)x100) into a total score between 0 (extreme difficulty) and 100 (no difficulty at all). Based on their WORQ scores at three months post-TKA, patients fall into one of three recovery groups (illustration 1):
- Early recovery (scores >70)
- Intermediate recovery (scores 51-70)
- Late recovery (scores <51)
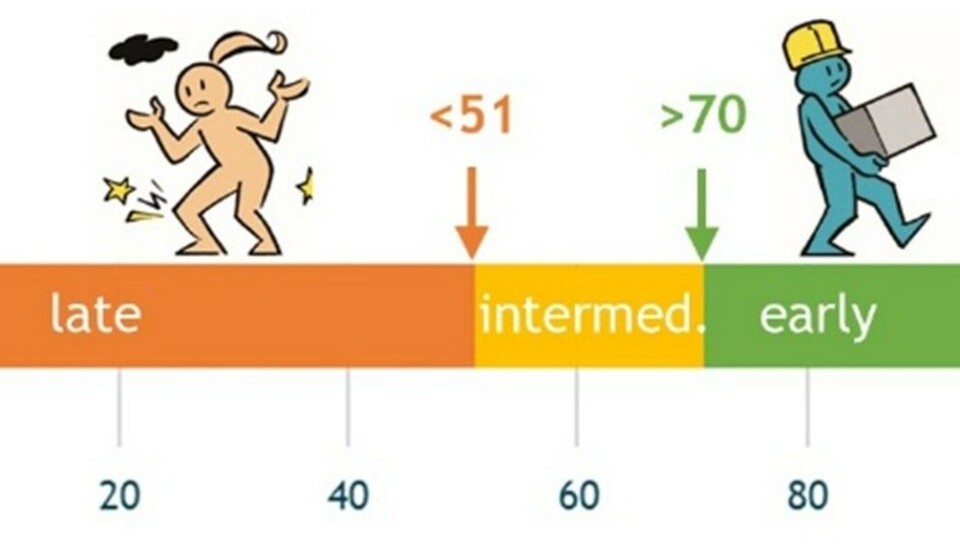
Illustration 1. WORQ-scores categorisation for early, intermediate and late of recovery groups.
This grouping is not just academic—it has real-world implications. The scores predict how well patients will be able to perform knee-straining work tasks at six and twelve months after surgery and how soon they will return to work. For physiotherapists, this tool provides a timely, reliable way to identify which patients might need more intensive or specialized rehabilitation focused on work-related goals.
Work ability and return to work after TKA
Patients with end-stage osteoarthritis of the knee face significant functional limitations before surgery. Everyday activities such as climbing stairs, walking on uneven surfaces, or kneeling can be painful or impossible. When these patients are of working age, which is increasingly common (4), these physical limitations naturally affect their ability to perform their job duties. Total knee arthroplasty is well known for reducing pain and improving general knee function in daily life, but its effect on specific work-related activities and return to work has been less clear (5).
In our prospective cohort study including 182 Dutch working patients receiving TKA, we used the WORQ to assess patients’ self-reported difficulty with work activities before surgery and at 3, 6, and 12 months after surgery. Those who scored ≤50 at 3 months—the late recovery group—continued to experience significant limitations in work-related activities even a year after surgery (Figure 1). Many in this group showed little or no clinically important improvement from their preoperative status. By contrast, patients in the early recovery group (WORQ ≥71) showed clinical meaningful improvement by 3 months, and those in the intermediate group caught up by 12 months. These differences translated into meaningful impacts on return to work. Late recovery patients returned to work roughly three weeks later (median 84 days) than early recovery patients did (62 days) —a delay with important consequences for patients’ well-being.
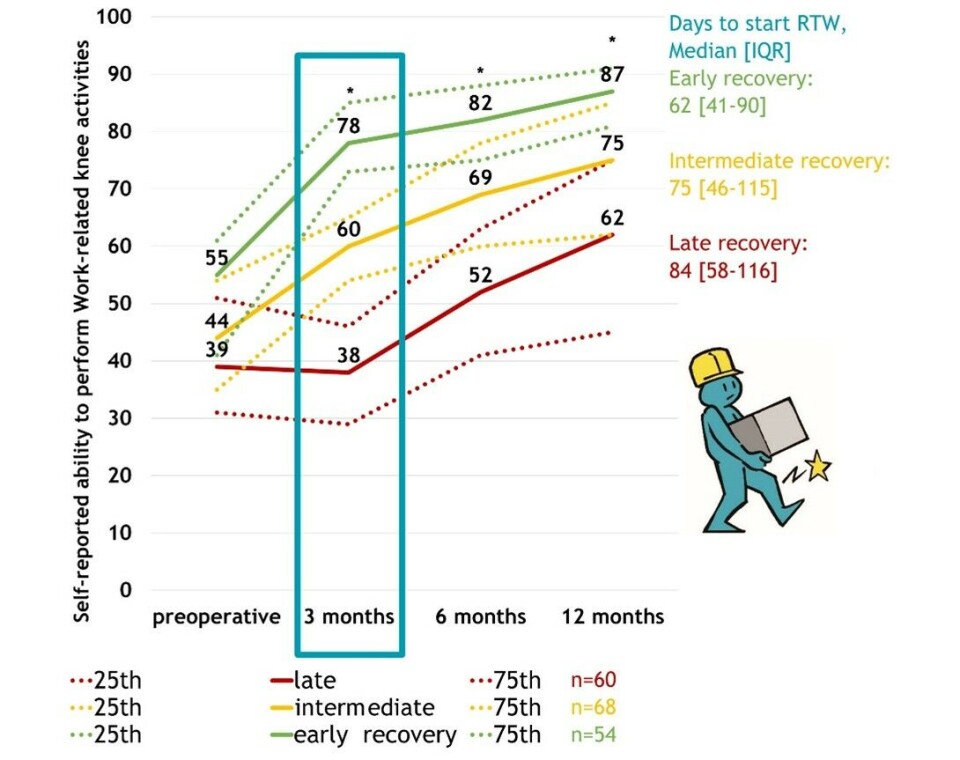
Figure 1. Recovery trajectories of ability to perform work-related activities (WORQ-score) and days to return to work in early, intermediate and late recovery groups of TKA patients.
The importance of patient expectations and pain management
Identifying which patients are most likely to fall into the late recovery group is essential for early intervention. Our study explored preoperative patient characteristics such as age, sex, body mass index, comorbidities, baseline knee pain, education level, and importantly, patients’ own expectations for recovery of work ability. Postoperative pain at 3 months was also measured, because of the limiting effect on recovery.
The strongest prognostic factors for belonging to one of the three recovery groups were patients’ expectations and their pain levels after surgery. Those who expected to experience less difficulty to resume work-related activities and reported less pain at 3 months post-TKA were more likely to belong to the early recovery group. These findings emphasize the critical role of managing patient expectations before surgery and controlling pain effectively afterward. Clear communication and education can help patients develop realistic goals (6, 7), potentially improving motivation and adherence to rehabilitation plans.
Practical implications for physiotherapists and (occupational) healthcare teams
For physiotherapists, the WORQ questionnaire offers more than just a number—it provides actionable insight into patients’ recovery trajectory and work ability. By administering the WORQ at three months post-TKA, therapists can categorize patients and tailor treatment plans accordingly.
Patients in the late recovery group may benefit from:
- Work-related goal setting during physiotherapy sessions (8)
- Early referral to occupational health specialists for workplace assessments and adjustments (9)
- Collaborative care involving clinical and occupational care (9, 10)
Additionally, physiotherapists can use WORQ scores to facilitate communication among healthcare providers, ensuring that everyone involved understands the patient’s work challenges and progress.
Patient education should be an integral part of care, especially focusing on realistic work-related expectations. While research specifically targeting work expectations after TKA is limited, existing evidence supports that managing expectations improves outcomes in general knee function and satisfaction.
Why This Matters
As the population ages, retirement age is increasing and the number of working-age patients receiving TKA increases (4), thereby the need to bridge clinical recovery and successful return to work becomes more pressing. Unaddressed work limitations can lead to prolonged absence, financial strain, and decreased quality of life.
Integrating the WORQ into routine clinical practice provides physiotherapists and healthcare teams with a validated, patient-centred tool to track recovery progress specifically related to work. This can facilitate earlier interventions, reduce delayed RTW, and ultimately improve patients’ physical and social well-being.
Conclusion
The WORQ questionnaire is a simple, effective way for physiotherapists to detect delayed work recovery early after total knee arthroplasty. By identifying patients at risk three months post-TKA, healthcare professionals can implement targeted rehabilitation strategies, set realistic goals, and coordinate multidisciplinary care to support a timely and successful return to work.
References
1. van Zaanen Y, Hoozemans MJM, Kievit AJ, Kuijer P, Expect TOwC. Predictive Validity of the Work, Osteoarthritis, or Joint Replacement Questionnaire for Return to Work After Total Knee Arthroplasty: A 12-Month Multicenter Prospective Cohort Study. J Arthroplasty. 2025;40(3):625-31.
2. Kievit AJ, Kuijer PP, Kievit RA, Sierevelt IN, Blankevoort L, Frings-Dresen MH. A reliable, valid and responsive questionnaire to score the impact of knee complaints on work following total knee arthroplasty: the WORQ. J Arthroplasty. 2014;29(6):1169-75 e2.
3. Gagnier JJ, Mullins M, Huang H, Marinac-Dabic D, Ghambaryan A, Eloff B, et al. A Systematic Review of Measurement Properties of Patient-Reported Outcome Measures Used in Patients Undergoing Total Knee Arthroplasty. J Arthroplasty. 2017;32(5):1688-97 e7.
4. Culliford D, Maskell J, Judge A, Cooper C, Prieto-Alhambra D, Arden NK, et al. Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthritis Cartilage. 2015;23(4):594-600.
5. Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, et al. Knee replacement. Lancet. 2018;392(10158):1672-82.
6. Tolk JJ, Janssen RPA, Haanstra TM, van der Steen MC, Bierma-Zeinstra SMA, Reijman M. The influence of expectation modification in knee arthroplasty on satisfaction of patients: a randomized controlled trial. Bone Joint J. 2021;103-B(4):619-26.
7. Churchill LG, J; Meaker, M; et al. Patient and Clinician Perceptions of a Clinical Decision Support Tool for Personalized Rehabilitation after Total Knee Arthroplasty: A Qualitative Interview Study. Preprint2023.
8. Hoorntje A, Waterval-Witjes S, Koenraadt KLM, Kuijer P, Blankevoort L, Kerkhoffs G, et al. Goal Attainment Scaling Rehabilitation Improves Satisfaction with Work Activities for Younger Working Patients After Knee Arthroplasty: Results from the Randomized Controlled ACTION Trial. J Bone Joint Surg Am. 2020;102(16):1445-53.
9. Kangas P, Soini S, Pamilo K, Kervinen V, Kinnunen ML. Return to Work Following Hip or Knee Arthroplasty: A One-Year Prospective Cohort Study in Participants with Direct Referral from Hospital to Occupational Health Care Services. J Occup Rehabil. 2024.
10. Strijbos DO, van der Sluis G, van Houtert WFC, Straat AC, van Zaanen Y, de Groot S, et al. Protocol for a multicenter study on effectiveness and economics of the Back At work After Surgery (BAAS): a clinical pathway for knee arthroplasty. BMC Musculoskelet Disord. 2023;24(1):199.





















