Fagfellevurdert

Management of Frozen Shoulder Using Corticosteroid Injection Therapy: An Evaluation of Current Practice among Physical Therapists Providing Injection Therapy in Norway
Vitenskapelig artikkel
Joakim Moestue Halvorsen, Forsterket rehabilitering Aker, Helseetaten, Oslo kommune, Oslo, Norway. joakim.halvorsen@outlook.com.
Nick Worth, University of Salford, Salford, GB and Queen Margaret University, Edinburgh, GB.
Cathy Bulley, Queen Margaret University, Edinburgh, GB.
This scientific article has been peer-reviewed according to Fysioterapeuten’s guidelines, and was accepted on November 2nd, 2021. Ethical approval was granted by the Queen Margaret University (QMU) Divisional Research Ethics Committee. No conflicts of interest stated.
Note: Moestue Halvorsen is associated with Fysioterapeuten in connection with the podcast "Lateralt og medialt – en podcast om fysioterapi”.
Abstract
Introduction: Although several interventions have been proposed for frozen shoulder, there is a lack of evidence regarding the best care for the condition, especially concerning corticosteroid treatment and the number of injections used. The treatment strategies and clinical reasoning behind the management among physical therapists providing injection therapy have not previously been evaluated.
Methods: A cross-sectional online survey was distributed among 138 Norwegian physical therapists providing injection therapy to evaluate current practice regarding their management of frozen shoulder with corticosteroid injections. Descriptive statistics were used to identify trends in current practice, which were further evaluated in relation to the available literature.
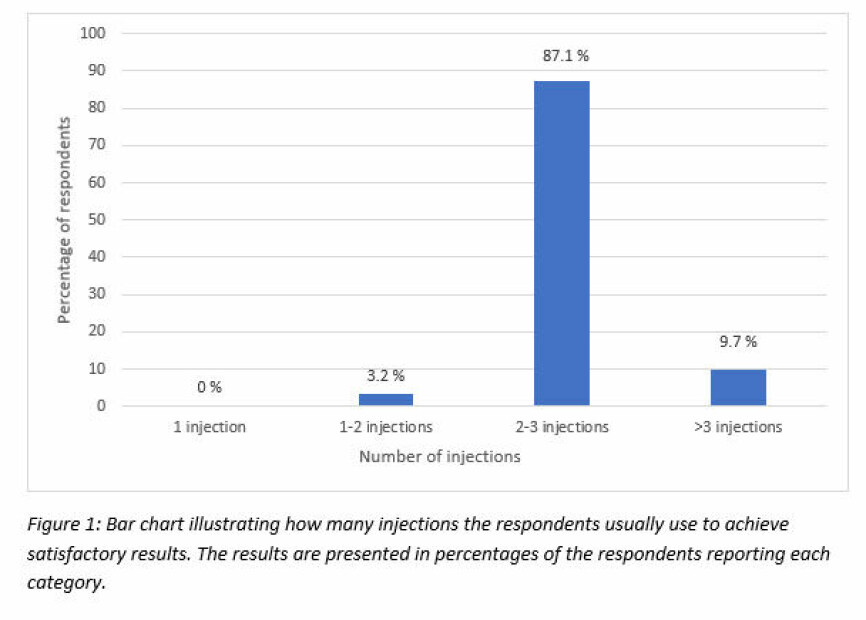
Results: The majority of the 32 respondents used multiple ultrasound-guided intra-articular corticosteroid injections for frozen shoulder. None reported to usually achieve satisfactory results following only a single injection, while 87.1 % reported this following 2-3 injections. The use of functional outcome measures as part of the evaluation and decision-making is generally limited among the respondents.
Conclusion: Multiple intra-articular corticosteroid injections are currently used in practice in Norway, with the respondents reporting beneficial outcomes following 2-3 injections. However, their efficacy compared to a single injection needs further investigation.
Key-words: Physical Therapy Modalities, Surveys and Questionnaires, Shoulder Injection.
Sammendrag
Behandling av frossen skulder med kortisoninjeksjon: En evaluering av nåværende praksis blant fysioterapeuter som utfører injeksjonsbehandling i Norge
Formål: Å evaluere nåværende praksis vedrørende bruk av kortisoninjeksjoner i behandlingen av frossen skulder blant fysioterapeuter som utfører injeksjonsbehandling i Norge, og undersøke i hvilken grad funksjonelle utfallsmål brukes som en del av evalueringen og beslutningsgrunnlaget for behandling.
Design: Nettbasert spørreundersøkelse
Materiale: Svar på den nettbaserte spørreundersøkelsen var tilgjengelig fra 32 fysioterapeuter som utfører injeksjonsbehandling i Norge.
Metode: Tverrsnittstudie
Resultater: Alle respondentene i denne spørreundersøkelsen benytter ultralydveiledet intraartikulær injeksjon ved behandling av frossen skulder med kortison. Alle respondentene anså kortisoninjeksjoner som hensiktsmessige i den smertedominerende fasen, med mer motstridende synspunkter om hvor hensiktsmessig slik behandling er i den stivhetsdominerende fasen. Alle unntatt én av respondentene rapporterte at de kan vurdere å benytte mer enn én injeksjon på samme side. Blant respondentene som benytter flere injeksjoner, rapporterte 87,1 % at de vanligvis oppnår et tilfredsstillende resultat ved 2-3 injeksjoner, mens ingen rapporterte at de vanligvis oppnår dette etter kun én injeksjon.
Respondentene benytter ofte selvrapportert grad av smerte med Visuell Analog Skala (VAS) eller Numeric Rating Scale (NRS) for å evaluere behandlingseffekt. Én av fem benytter også et funksjonelt utfallsmål, mens ingen rapporterte å benytte et mål for helserelatert livskvalitet.
Konklusjon: Flere intraartikulære kortisoninjeksjoner brukes i dag i behandlingen av frossen skulder av fysioterapeuter som utfører injeksjonsbehandling i Norge, med rapporter fra respondentene om tilfredsstillende resultater etter 2-3 injeksjoner. Bruk av funksjonelle utfallsmål til evaluering og som en del av beslutningsgrunnlaget for behandling skjer kun i begrenset grad.
Nøkkelord: Fysioterapi, undersøkelser og spørreskjemaer, skulder, injeksjoner.
Introduction
Frozen shoulder is a debilitating condition identified by severe pain and stiffness of the shoulder and has been associated with reduced quality of life among individuals living with the condition (1). Although it can be secondary to trauma or prolonged immobilization, primary frozen shoulder is seen as an idiopathic process marked by initial inflammation and subsequent fibrosis, capsular contracture, and reduced joint volume (2, 3). Since the seminal paper by Reeves (4) in 1975 on the natural history of frozen shoulder, the condition has been thought of as self-limiting, leading to full resolution without treatment after one to three years. However, a recent systematic review by Wong et al. (5) found that the condition could still cause symptoms and disability several years after onset.
Frozen shoulder has traditionally been reported to occur in 2-5 % of the general population, although there are uncertainties regarding the actual life-time prevalence of the condition (3). As the incidence of frozen shoulder peaks in the fifth and sixth decade, a high proportion of the patients are in the working population, leading to a substantial economic burden to both the individual and the society (6). In addition to costs accumulating from the loss of workdays, the healthcare system's cost from treatments of frozen shoulder is substantial (7).
Although there is no Norwegian national guideline dictating the care and interventions that should be provided for frozen shoulder, clinical practice guidelines for the management of the condition have been developed for physical therapists both in Norway (8), and abroad (9, 10).
To help guide clinicians with decision-making and to identify appropriate interventions, a dichotomization between the "pain-predominant" and the "stiffness-predominant" stage of the disease has been recommended. Inflammation is the hallmark of the former, while capsular contracture is thought to be the most notable feature in the latter (9). A vast number of interventions has been proposed for the different stages of frozen shoulder, ranging from conservative management such as education and advice, supervised neglect, exercise therapy, stretching, joint mobilization and manipulation, through minimally invasive procedures like acupuncture and injection therapy, and finally to surgical treatment such as capsular release (3, 9). In a survey of 289 physiotherapists in the United Kingdom, good agreement was observed for certain interventions in both pain-predominant and stiffness-predominant frozen shoulder. Advice and education were recognized as essential interventions in both stages. There was also good agreement on the use of corticosteroid injection therapy in pain-predominant frozen shoulder, with 80 % of the respondents regarding it appropriate (11). Although the indications for corticosteroid injections in musculoskeletal care in general are narrow, and the effects often short-lived (12), several systematic reviews supports this intervention in frozen shoulder (13, 14). Intra-articular injection of corticosteroid is also recommended in the pain-predominant stage in the clinical practice guidelines for frozen shoulder. However, the guidelines do not specify the number of injections considered appropriate (8-10). Many researchers suggest using a single corticosteroid injection for frozen shoulder (2, 15, 16), while others have advocated the use of multiple injections (17-19). In their systematic review, Shah and Lewis (20) concluded that there is evidence of benefit using one to three intra-articular corticosteroid injections with limited evidence of using up to six injections for frozen shoulder.
Even though the survey by Hanchard et al. (11) identified that corticosteroid injection therapy is regarded appropriate for pain-predominant frozen shoulder by the responding physical therapists, it does not investigate the decision-making and actual management of the condition, as the majority of the respondents (76 %) did not practice injection therapy themselves. However, the finding is comparable to the results from several evaluations among practitioners of the medical profession, where corticosteroid injection has been reported among the most commonly used interventions for frozen shoulder (21-23). As none of these practice evaluations differentiated between single- and multiple corticosteroid injections, it is not known to what extent multiple corticosteroid injections are perceived as appropriate and used in current clinical practice.
In addition to guide interventions, the clinical practice guidelines recommend physical therapists to use validated functional outcome measures like the Shoulder Pain and Disability Index (SPADI) or the Disabilities of the Arm, Shoulder and Hand (DASH) when monitoring change in patients with frozen shoulder (8-10). There is limited data in the identified practice evaluations to inform whether, and to what extent, validated functional outcome measures are currently used by clinicians when treating frozen shoulder with corticosteroid injections.
There are currently few countries where physical therapists can use injection therapy as part of their scope of practice. In Norway this treatment is only provided by physical therapist when acting as an aid to a physician, as Norwegian physical therapists are not independent prescribers of corticosteroids or other injectable drugs. The practice is also quite new, and was just recently endorsed by the Norwegian Physiotherapist Association (NPA/NFF). As physical therapists acquire new tools for treatment such as injection therapy, it is essential to evaluate how they are used in clinical practice. Establishing how injection therapy is commonly used by physical therapists when treating frozen shoulder may give insight into how the current practice compares to the available evidence on the topic, and potentially give evidence to update current working practices or future research priorities. While investigating this, it would also be relevant to establish whether the reported improvements from clinicians are based on validated functional outcome measures, as clinical practice guidelines for frozen shoulder recommend using validated functional outcome measures to evaluate progress (8-10).
Aims and objectives
This research project aims to evaluate the management of frozen shoulder among Norwegian physical therapists providing injection therapy, and compare the results to the existing evidence on the subject.
Primary objective: Evaluate the current use of corticosteroid injection therapy for frozen shoulder among physical therapists providing injection therapy in Norway.
Secondary objectives: Investigate to what extent validated functional outcome measures are used as part of the evaluation and decision-making in the treatment of frozen shoulder among the same practitioners.
Methods
To evaluate the current practice regarding corticosteroid injection therapy for frozen shoulder among physical therapists providing injection therapy in Norway, a cross-sectional online survey was developed and distributed to eligible practitioners. The survey research design was chosen as this allows for distribution to a large cohort of the targeted population and permits quantification of the individual responses so that a description of the current practice in the sample can be made.
The survey was developed in Bristol Online Survey by the primary author. The aims of the survey were: (a) to identify what injection techniques and drugs that are commonly used; (b) to identify the respondents' attitudes towards providing single- and multiple corticosteroid injections for frozen shoulder; (c) to identify the respondents' treatment strategies and perceived benefits if providing multiple injections; and (d) to identify to what extent validated functional outcome measures are used as part of the evaluation and decision-making in the treatment of frozen shoulder among the respondents.
Careful planning went into the survey's development and design, ensuring that each question would provide information relating to one of the survey aims. The survey was piloted on a group of three eligible participants with minor alterations made based on the sample population's feedback.
Prior to the distribution of the survey, ethical approval was granted by the Queen Margaret University (QMU) Divisional Research Ethics Committee. In addition, a “Fremleggsvurdering” was sent to Regionale Komiteer for Medisinsk og Helsefaglig Forskningsetikk (REK). The “Fremleggsvurdering” was returned by the REK committee on the 5th of February 2020, who decided that the project would not need to undergo additional ethical review in Norway.
The recruitment of participants was done through advertising in a Norwegian special interest group (SIG) for injection therapy on Facebook. The survey was open and available for responses from the 29th of March until the 30th of April 2020. At the time of distribution, the SIG had 200 active members, of whom 139 (including the primary author) are physical therapists.
All data were collected anonymously, and respondents were informed of the option to omit answering questions, and the possibility to withdraw consent at any time during the survey. Inclusion criteria for participation were: Being a physical therapist providing injection therapy for frozen shoulder in the primary care or private practice in Norway and consenting to participate in the online survey. The only exclusion criteria was that they had not previously treated patients with frozen shoulder using injection therapy.
Data management and analysis
The raw data from the survey were collected and stored in the Bristol Online Survey (BOS) server and downloaded to a password-protected QMU server. The data was then exported to Microsoft Excel for Microsoft 365 MSO (16.0.13127.20402) 64-bit for further analysis.
Frequency counts and descriptive analysis were made for responses to all questions. Considering that this study's primary aim was to evaluate the current use of corticosteroid injection therapy for frozen shoulder among physical therapists providing injection therapy in Norway, descriptive analysis of the responses serves the purpose of identifying the essence of the current practice in the sample. This allows for a comparison between the current practice and the available literature.
The analysis function integrated in BOS was used to count frequencies and calculate percentages on the closed-ended questions. Response categories were made for answers given in the open response fields. The answers were manually categorized for similar meaning by the primary author, and the frequencies of responses in each category are reported to quantify the answers. The figure presented was made using Microsoft Excel.
Results
The online survey returned 32 responses among the 138 physical therapists (excluding the primary author) that were members of the SIG at the time the survey was open for participation, giving a response rate of 23.2 % (32/138). Presented are the frequencies of responses to each question in the survey.
Question 1: What type of corticosteroid injection (localization) do you use to treat frozen shoulder?
All 32 respondents (100 %) reported using intra-articular localization of the injection when treating frozen shoulder. None of the respondents reported using subacromial injection or injection into the rotator interval for frozen shoulder.
Question 2: What technique do you utilize most for administering injection therapy for frozen shoulder?
All 32 respondents (100 %) reported using ultrasound guidance when administering injection therapy for frozen shoulder. None of the respondents reported only using an anatomically guided technique.
Question 3: Do you consider corticosteroid injections to be suitable for treating frozen shoulder in:
- The pain-predominant stage
- The stiffness-predominant stage
All 32 respondents (100 %) reported that they consider corticosteroid injections suitable when treating frozen shoulder in the pain-predominant stage. Twelve respondents (37.5 %) also considered it appropriate in the stiffness-predominant stage, although four of them specified in the open response field that this only applied if the patient still experienced pain.
Question 4: Would you consider administering more than a single corticosteroid injection at the same side for frozen shoulder?
31 respondents (96.9 %) reported to consider administering multiple corticosteroid injections for frozen shoulder. Only one respondent (3.1 %) reported not to consider administering more than a single injection.
Question 4.1: How many corticosteroid injections do you normally administer to achieve satisfactory results?
None of the respondents reported to normally achieve satisfactory results following only a single corticosteroid injection, and one respondent (3.2 %), using the open response field, reported to normally achieve satisfactory results following 1-2 corticosteroid injections. Twenty-seven respondents (87.1 %) reported that they normally achieve satisfactory results following 2-3 corticosteroid injections, while three respondents (9.7 %) reported to normally administer > 3 corticosteroid injections before achieving satisfactory results. The responses to question 4.1 are illustrated in Figure 1.
Question 4.2: What do you consider the most important criteria to guide whether to repeat the injection or not?
Twenty respondents (64.5 %) answered that they consider persistent pain reported by the patient to be the most important factor to guide when to provide a repeated injection. Ten respondents (32.3 %) reported persistent pain on clinical assessment to be the most important criteria for administering a repeated injection, while one respondent (3.23 %) reported initial severity as the most important criteria. Analysis of the open-response field revealed that two respondents who selected "persistent pain" also considered "clinical assessment" equally important. Adding these responses brings the total number of respondents reporting "clinical assessment" to 12, giving a percentage of 38.7 %. In addition, one respondent reported taking improvement after the previous injection into account when considering to repeat the injection.
Question 5: How do you usually monitor progression/treatment effect in patients with frozen shoulder?
Twenty-nine respondents (90.6 %) reported using the clinical assessment to monitor the progression/treatment effect. Twenty respondents (62.5 %) reported using subjective measures to evaluate the progression/treatment effect, with one relying solely on this. Objective outcome measures were reported used by 15 respondents, with one more identified from the open response field, bringing the total to 16 respondents (50 %). Nine respondents (28.1 %) reported using a combination of the three evaluation options.
Question 5.1: What types of objective outcome measures do you usually use for patients with frozen shoulder?
13 respondents (41.9 %) reported using the Visual Analog Scale (VAS), and 12 respondents (38.7 %) reported using the Numeric Rating Scale/Numeric Pain Rating Scale (NRS/NPRS), with three of these respondents reporting using both. The Shoulder Pain and Disability Index (SPADI) was reported used by five respondents (16.1 %), and the Simple Shoulder Test (SST) was reported used by one respondent (3.23 %). None of the respondents reported using any of the listed measures for health-related quality of life (36-Item Short Form Health Survey or the EQ-5D).
Discussion
This study describes the current practice regarding corticosteroid injection therapy for frozen shoulder in a sample of Norwegian physical therapists providing injection therapy. The sample was recruited from a Norwegian SIG for injection therapy on Facebook, with a response rate of 23.2 %. Compared to previous surveys of practitioners managing frozen shoulder, this survey had a lower response rate than achieved by Kraal et al. (22) in 2016 (54 %) and by Randelli et al. (23) in 2012 (40 %), but was comparable to the results obtained by Buchbinder et al. (21) in 2013 (17.5 % among general practitioners and 23.8 % among rheumatologists). Recognizing the variability in response rates to web-based surveys and response rates in similar populations, the response rate achieved in this study seems acceptable to evaluate the current practice among physical therapists providing injection therapy in Norway.
The results of this survey indicate that the respondents are uniform in how the procedure is performed. All respondents reported using ultrasound-guided intra-articular injections when treating frozen shoulder using corticosteroids. The use of intra-articular placement of the corticosteroid is in line with systematic reviews (13, 14) and clinical practice guidelines (8-10). There is a paucity of studies investigating the added value and cost-effectiveness of performing the injections under ultrasound guidance, although studies investigating accuracy shows a higher rate of successful intra-articular placement of the drug when using ultrasound-guidance compared to an anatomically guided technique (24, 25). The same studies also demonstrated more significant improvements in pain and range of motion following a single ultrasound-guided injection in the short term, but the results following the anatomically guided technique were comparable after the initial few weeks after the injection. Even though conclusive evidence of superiority is lacking, the current practice in this sample of performing the injections using ultrasound-guidance seems justified.
There was a complete agreement among the respondents on the appropriateness of using corticosteroid injections in the pain-predominant stage, with more conflicting views regarding appropriateness in the stiffness-predominant stage. This result is comparable to previous surveys performed among other healthcare providers, where injection therapy is often preferred in the pain-predominant stage of frozen shoulder, but to a lesser extent in the stiffness-predominant stage (11, 22, 23). Although there has been reports of potential harmful effects of corticosteroid injections, especially when used in tendinopathies (26), their use when treating frozen shoulder in primary care has been considered useful and safe, with few and minor side effects (27). This samples views on providing corticosteroid injections in the pain-predominant stage is in accordance with clinical practice guidelines (8-10).
In this sample, 96.9 % of the respondents reported that they would consider administering multiple corticosteroid injections for frozen shoulder. This constitutes a substantial proportion of the respondents, considering that there is a gap in the published literature to guide clinicians whether to provide a single- or multiple corticosteroid injections when treating patients with frozen shoulder. Although the effectiveness of providing multiple corticosteroid injections for frozen shoulder have been advocated both in a systematic review (20) and several subsequent randomized controlled trials (RCTs) (28-33), none of the RCTs published to date have investigated the effects of multiple corticosteroid injections compared to a single corticosteroid injection. This means that the results of these studies cannot be used to infer whether multiple injections are in fact superior to a single injection.
Interestingly, among the respondents using multiple injections, none reported that they usually achieve satisfactory results following only a single injection. This lack of perceived satisfactory results following a single corticosteroid injection is striking, given that this is the treatment strategy that is most commonly investigated in research on corticosteroid injections for frozen shoulder. In contrast, 87.1 % of the respondents reported achieving satisfactory results following 2-3 injections, a treatment strategy that is far less used in research studies. When interpreting these results, it is important to note that the term "satisfactory results" was not explicitly defined. Therefore, it might be variability in what criteria that makes the individual respondents perceive a “satisfactory result” following the treatment. It is also not known to whom the result is perceived satisfactory, the patient or the clinician. The finding that the majority of the respondents in this sample uses multiple corticosteroid injections, a treatment strategy that has not been properly explored in controlled research studies, implicates that further investigation of this intervention could be warranted. Evaluating the efficacy of multiple injections was also identified as a research priority in a large systematic review and cost-effectiveness analysis regarding the management of frozen shoulder (2).
Regarding objective outcome measures to evaluate treatment effect, patient-reported outcome measures (PROMs) regarding pain level using the VAS or NRS were most commonly used. Less than one in five of the respondents (19.4 %) reported using a functional outcome measure to evaluate treatment effect, while none reported using a measure of health-related quality of life. Validated functional outcome measures and measures of health-related quality of life are increasingly encouraged in the care of musculoskeletal conditions (34), and the use of functional outcome measures are recommended in clinical practice guidelines when treating patients with frozen shoulder (8-10). The results of this survey demonstrate that the respondents rely on clinical assessment and subjective measures, including the PROMs regarding level of pain, when evaluating treatment effect, with only a small portion of the respondents using functional outcome measures routinely. This finding indicates that the majority of the respondents in this sample are not adhering to recommendations in the clinical practice guidelines regarding the evaluation of treatment effect.
As there is a limited number of physical therapists providing injection therapy in Norway, the sample of respondents is small and might be susceptible to responder bias. However, the respondents are quite uniform regarding several of the important findings, which increases the credibility of the results. Another limitation to this study is not providing information regarding drugs and dosages used by the sample. Although it is the physician that is responsible for prescribing the appropriate drug and dosage, it could be argued that the physical therapists might still influence the physician’s choice. This makes it important for physical therapists to always recommend the lowest efficient dose, as it might decrease side-effects of the treatment. Even though providing intra-articular corticosteroid injections for frozen shoulder is supported by current evidence (13, 14), other interventions are also recommended in the clinical practice guidelines (8-10). Investigating concurrent use of these interventions could provide further insight into the physical therapist’s adherence to the clinical practice guidelines. However, evaluating the use of concurrent interventions was outside the scope of this evaluation.
As multiple injections have received little attention compared to the extent they are used in clinical practice when treating frozen shoulder in Norway, this treatment strategy might warrant further investigation in controlled research studies to establish its effectiveness compared to a single corticosteroid injection.
Conclusion
This study has evaluated the current practice regarding corticosteroid injection therapy for frozen shoulder in a sample of Norwegian physical therapists providing injection therapy, and found that the majority of the sample provides multiple ultrasound-guided intra-articular corticosteroid injections. Among the respondents using multiple injections, 87.1 % reported achieving satisfactory results following 2-3 injections, while none reported to usually achieve satisfactory results following only a single injection.
The use of functional outcome measures is generally limited among the respondents, and interventions should be initiated to implement these measures into routine practice to ensure adherence to clinical practice guidelines.
Acknowledgements: The authors would like to thank Martin Moum Hellevik, Anne-Marthe Sanders, Magnus Brekke and Simen Klunderud for valuable feedback and input in the process of writing this manuscript.
References
1. Fernandes MR. Correlation between functional disability and quality of life in patients with adhesive capsulitis. Acta ortopedica brasileira 2015; 23: 81-84. https://www.doi.org/10.1590/1413-78522015230200791 [doi].
2. Maund E, Craig D, Suekarran S, et al. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health technology assessment (Winchester, England) 2012; 16: 1-264. https://www.doi.org/10.3310/hta16110 [doi].
3. Lewis J. Frozen shoulder contracture syndrome - Aetiology, diagnosis and management. Manual therapy 2015; 20: 2-9. https://www.doi.org/10.1016/j.math.2014.07.006 [doi].
4. Reeves B. The natural history of the frozen shoulder syndrome. Scandinavian journal of rheumatology 1975; 4: 193-196. https://www.doi.org/10.3109/03009747509165255 [doi].
5. Wong CK, Levine WN, Deo K, et al. Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy 2017; 103: 40-47. S0031-9406(16)30030-X [pii].
6. Rangan A, Goodchild L, Gibson J, et al. Frozen Shoulder. Shoulder & elbow 2015; 7: 299-307. https://www.doi.org/10.1177/1758573215601779 [doi].
7. van den Hout WB, Vermeulen HM, Rozing PM, et al. Impact of adhesive capsulitis and economic evaluation of high-grade and low-grade mobilisation techniques. The Australian journal of physiotherapy 2005; 51: 141-149. S0004-9514(05)70020-9 [pii].
8. Haldorsen B, Røe Y, Thornes E, et al. Frossen skulder - fysioterapi. Helsebiblioteket.no 2018.
9. Hanchard N, Goodchild L, Thompson J, et al. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder v.1.7, “standard” physiotherapy. Endorsed by the Chartered Society of Physiotherapy 2011.
10. Kelley MJ, Shaffer MA, Kuhn JE, et al. Shoulder pain and mobility deficits: adhesive capsulitis. The Journal of orthopaedic and sports physical therapy 2013; 43: A1-31. https://www.doi.org/10.2519/jospt.2013.0302 [doi].
11. Hanchard NC, Goodchild L, Thompson J, et al. A questionnaire survey of UK physiotherapists on the diagnosis and management of contracted (frozen) shoulder. Physiotherapy 2011; 97: 115-125. https://www.doi.org/10.1016/j.physio.2010.08.012 [doi].
12. Cato RK. Indications and Usefulness of Common Injections for Nontraumatic Orthopedic Complaints. Med Clin North Am 2016; 100: 1077-1088.
13. Challoumas D, Biddle M, McLean M, et al. Comparison of Treatments for Frozen Shoulder: A Systematic Review and Meta-analysis. JAMA Netw Open 2020; 3.
14. Sun Y, Zhang P, Liu S, et al. Intra-articular Steroid Injection for Frozen Shoulder: A Systematic Review and Meta-analysis of Randomized Controlled Trials With Trial Sequential Analysis. The American Journal of Sports Medicine 2017; 45: 2171-2179. https://www.doi.org/10.1177/0363546516669944 [doi].
15. Carette S, Moffet H, Tardif J, et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo-controlled trial. Arthritis and Rheumatism 2003; 48: 829-838. https://www.doi.org/10.1002/art.10954 [doi].
16. Sun Y, Lu S, Zhang P, et al. Steroid Injection Versus Physiotherapy for Patients With Adhesive Capsulitis of the Shoulder: A PRIMSA Systematic Review and Meta-Analysis of Randomized Controlled Trials. Medicine 2016; 95: e3469. https://www.doi.org/10.1097/MD.0000000000003469 [doi].
17. Atkins E, Kerr J and Goodlad E. A practical approach to orthopaedic medicine: assessment, diagnosis and treatment. 4th ed. ed.: Churchill Livingstone Elsevier, 2015.
18. Ombregt L. A system of orthopaedic medicine. 3rd ed. ed.: Churchill Livingstone Elsevier, 2013.
19. Saunders S and Longworth S. Injection techniques in musculoskeletal medicine: a practical manual for clinicians in primary and secondary care. 5th ed. ed. Edinburgh: Churchill Livingstone Elsevier, 2018.
20. Shah N and Lewis M. Shoulder adhesive capsulitis: systematic review of randomised trials using multiple corticosteroid injections. The British journal of general practice : the journal of the Royal College of General Practitioners 2007; 57: 662-667.
21. Buchbinder R, Staples MP, Shanahan EM, et al. General practitioner management of shoulder pain in comparison with rheumatologist expectation of care and best evidence: an Australian national survey. PloS one 2013; 8: e61243. https://www.doi.org/10.1371/journal.pone.0061243 [doi].
22. Kraal T, Visser C, Sierevelt I, et al. How to treat a frozen shoulder? A survey among shoulder specialists in the Netherlands and Belgium. Acta Orthopaedica Belgica 2016; 82: 78-84.
23. Randelli P, Arrigoni P, Cabitza F, et al. Current practice in shoulder pathology: results of a web-based survey among a community of 1,084 orthopedic surgeons. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 2012; 20: 803-815. https://www.doi.org/10.1007/s00167-011-1673-z [doi].
24. Lee HJ, Lim KB, Kim DY, et al. Randomized controlled trial for efficacy of intra-articular injection for adhesive capsulitis: ultrasonography-guided versus blind technique. Archives of Physical Medicine and Rehabilitation 2009; 90: 1997-2002. https://www.doi.org/10.1016/j.apmr.2009.07.025 [doi].
25. Raeissadat SA, Rayegani SM, Langroudi TF, et al. Comparing the accuracy and efficacy of ultrasound-guided versus blind injections of steroid in the glenohumeral joint in patients with shoulder adhesive capsulitis. Clinical rheumatology 2017; 36: 933-940. https://www.doi.org/10.1007/s10067-016-3393-8 [doi].
26. Coombes BK, Bisset L Fau - Vicenzino B and Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 2010; 376: 1751-1767.
27. Koh KH. Corticosteroid injection for adhesive capsulitis in primary care: a systematic review of randomised clinical trials. Singapore Med J 2016; 57: 646-657.
28. De Carli A, Vadalà A, Perugia D, et al. Shoulder adhesive capsulitis: manipulation and arthroscopic arthrolysis or intra-articular steroid injections? International orthopaedics 2012; 36: 101-106. https://www.doi.org/10.1007/s00264-011-1330-7 [doi].
29. Jacobs LG, Smith MG, Khan SA, et al. Manipulation or intra-articular steroids in the management of adhesive capsulitis of the shoulder? A prospective randomized trial. Journal of shoulder and elbow surgery 2009; 18: 348-353. https://www.doi.org/10.1016/j.jse.2009.02.002 [doi].
30. Lorbach O, Anagnostakos K, Scherf C, et al. Nonoperative management of adhesive capsulitis of the shoulder: oral cortisone application versus intra-articular cortisone injections. Journal of shoulder and elbow surgery 2010; 19: 172-179. https://www.doi.org/10.1016/j.jse.2009.06.013 [doi].
31. Schydlowsky P, Szkudlarek M and Madsen OR. Treatment of frozen shoulder with subcutaneous TNF-alpha blockade compared with local glucocorticoid injection: a randomised pilot study. Clinical rheumatology 2012; 31: 1247-1251. https://www.doi.org/10.1007/s10067-012-1993-5 [doi].
32. Sharma SP, Bærheim A, Moe-Nilssen R, et al. Adhesive capsulitis of the shoulder, treatment with corticosteroid, corticosteroid with distension or treatment-as-usual; a randomised controlled trial in primary care. BMC musculoskeletal disorders 2016; 17: 232-016-1081-1080. https://www.doi.org/10.1186/s12891-016-1081-0 [doi].
33. Tveitå EK, Tariq R, Sesseng S, et al. Hydrodilatation, corticosteroids and adhesive capsulitis: a randomized controlled trial. BMC musculoskeletal disorders 2008; 9: 53-2474-2479-2453. https://www.doi.org/10.1186/1471-2474-9-53 [doi].
34. Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. British journal of sports medicine 2020; 54: 79-86. https://www.doi.org/10.1136/bjsports-2018-099878 [doi].
© Author(s) (or their employer(s)) 2021. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions (https://creativecommons.org/licenses/by-nc/4.0/). Published by Fysioterapeuten.





















